20 September 2022 | News, Science
Iron deficiency in IBD, celiac disease and obesity

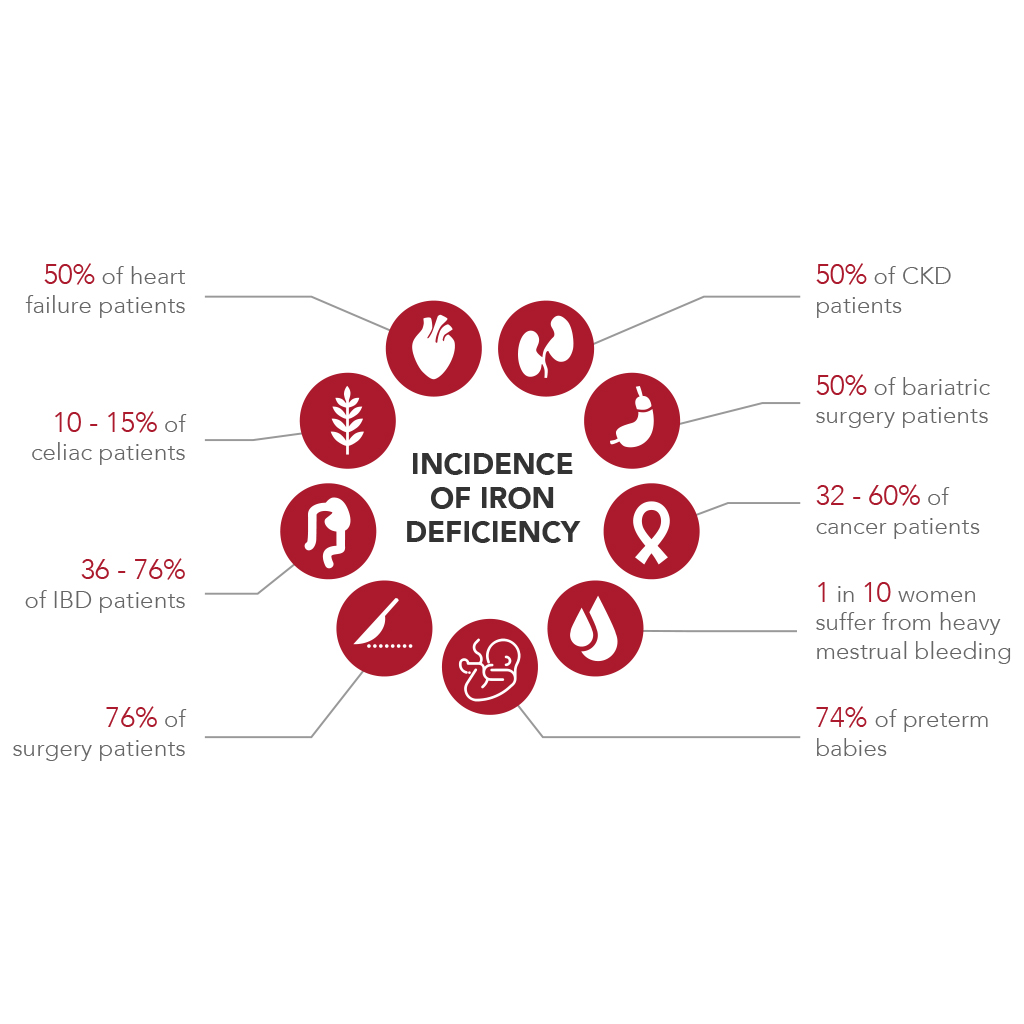
Many gastrointestinal diseases cause iron deficiency (sideropenia), which if not corrected can easily lead to iron deficiency anemia. The incidence of iron deficiency in gastroenterology is found in 10-15% of subjects suffering from celiac disease, this percentage rises to 50% of subjects undergoing bariatric surgery, while sideropenia is found in a wide range (36-76%) in subjects with inflammatory bowel diseases (IBD).
According to the World Health Organization (WHO) the physiological range of hemoglobin (Hb) varies according to gender and age: men 14-18 g/dL, women 12-16 g/dL and children 10,5-13,5 g/dL.
When Hb level is lower than the above values, we speak of iron deficiency anemia, which is also confirmed by the measurement of other important parameters:
- Ferritin, storage protein capable of containing up to 4500 iron atoms (physiological range: 30-300 ng/mL);
- Sideremia, which indicates the amount of iron in the bloodstream bound to a specific protein, called transferrin (physiological range: 50-180 mcg/dL);
- Saturation of transferrin (%TSAT), a protein that transports iron in the tissues and districts responsible for its use (physiological value: >20%).
In case of iron deficiency, instead, there are not always hematological alterations; in fact, hemoglobin levels may be normal, but ferritin and transferrin saturation are low.
Gastrointestinal diseases can lead to chronic inflammation, limiting the absorption and use of iron by the body; in fact, these patients have a functional sideropenia (Transferrin Saturation TSAT < 20% Ferritin >30 ng / mL), but conventional oral iron supplementation, usually, is not able to solve this problem, because in these chronic conditions, the body produces high levels of hepcidin, a peptide hormone produced by the liver, which works by reducing the serum concentration of iron
Celiac disease
Celiac disease is an autoimmune and small intestine disease caused by a hypersensitivity to the gliadin fraction of gluten, a cereal protein found in wheat, rye, and smaller quantities, barley, and oats. In these subjects, gliadin acts as a foreign agent which, not being recognized by the intestinal mucosa, promotes the aggregation of lymphocytes, and these cause damage to the intestinal mucosa which in turn degenerates until the intestinal villi disappear.
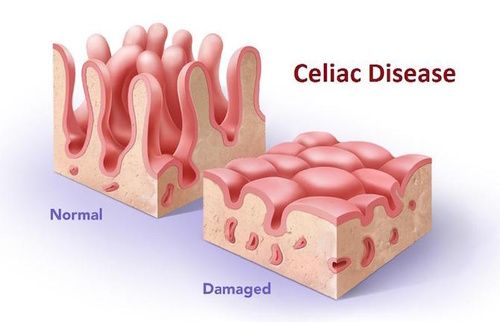
Source: https://www.cure-naturali.it/enciclopedia-naturale/salute/naturopatia/celiachia.htmlThe symptoms are varied from subject to subject and among the main ones we can find: diarrhea or constipation, bleeding, abdominal pain, loss of weight, skin rash, joint pain, headache, fatigue and iron deficiency anemia.
Inflammatory bowel diseases
Inflammatory Bowel Diseases (IBD) include ulcerative colitis and Crohn’s disease.
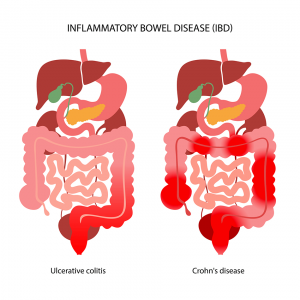
Source: https://www.hopkinsmedicine.org/health/conditions-and-diseases/inflammatory-bowel-disease
The symptoms that characterize Crohn’s disease and ulcerative colitis are generally different:
- Crohn’s disease most commonly affects the end of the small intestine and the beginning of the colon, but it can occur in any part of the gastrointestinal tract irregularly. In most cases, Crohn’s disease initially manifests itself with diarrhea and abdominal pain localized especially in the lower right part of the abdomen, which corresponds to the tract of the intestine in which the disease is most frequently located.
- Ulcerative colitis usually originates in the rectum but can extend continuously and involve the entire colon. It almost always manifests itself with diarrhea and the presence of blood and mucus in the stool, which is often associated with a feeling of incomplete evacuation and anemia.
In the phases of exacerbation of IBD can appear states of general malaise such as weight loss, fatigue, loss of appetite and fever. The European Crohn’s and Colitis Organisation (ECCO) has published guidelines, in which is specificated that to counter iron deficiency in patients suffering from these gastrointestinal diseases it is necessary to either resort to supplementation with iron-based products, or in severe cases to intravenous iron infusion.
Obesity
Obesity is one of the World’s biggest public health problems. Obese patients who cannot lose weight are increasingly resorting to bariatric surgery. All bariatric surgery techniques lead to a significant reduction in nutrient absorption. Iron, vitamin D and vitamin B12 are the main nutrients that are deficient after bariatric surgery.
SiderAL®: Sucrosomial® iron
To counter states of iron deficiency, PharmaNutra spa has developed Sucrosomial® Iron (SiderAL®). This new technology represents an innovative oral formulation containing iron, in which iron pyrophosphate is covered in a matrix of phospholipids and sucrose esters of fatty acids (Sucrosome®).
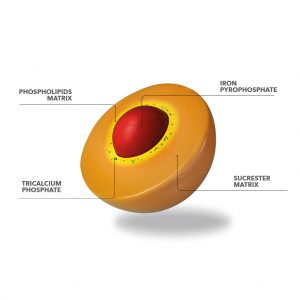
The result of this technology leads to high gastrointestinal tolerability and easier absorption of iron in the intestine. In recent years many scientific evidences (both preclinical and clinical) have been published in international scientific journals that confirm the effectiveness of Sucrosomial® Technology.
Gastroresistance is given by the sucrester matrix, as demonstrated in dedicated studies, which protects iron from the acidity of the pH of the stomach. This allows the Sucrosome® to reach intact in the intestinal mucosa, where it is absorbed by enterocytes as a vesicular structure through paracellular and transcellular pathways.
In the intestinal mucosa, in addition to enterocytes, there are membranous cells (M cells) belonging to Peyer’s plaques. Preclinical research studies have shown that these cells are also able to absorb the Sucrosome® by endocytosis.
Many clinical studies in the gastroenterological field with SiderAL® have allowed to demonstrate how this technology is able to restore normal hematochemical values and to guarantee the normal functionality of red blood cells and hemoglobin.
Conclusion
The innovation of Sucrosomial® Technology is characterized by excellent tolerability and allows the intake of iron at any time of the day (with the meal or away from meals), for long periods of time, and prevents any discomfort commonly associated with iron intake, such as unpleasant metallic aftertaste, irritation of the gastric mucosa, nausea, or constipation. Overcoming the limits related to conventional iron supplementation, SiderAL® promotes the intake of this important nutrient in all situations of deficiency or increased iron needs.
BIBLIOGRAPHY
- Sideral.it
- Humanitas.it/malattie/obesita
- Mici360.it/anemia-e-carenza-di-ferro-nella-malattia-di-Crohn
- Ecco-ibd.eu/publications/ecco-guidelines-science
- Gómez-Ramírez, E. Brilli, G. Tarantino, M. Muñoz, “Sucrosomial® Iron: A New Generation Iron for Improving Oral Supplementation,” Pharmaceuticals (Basel).2018 Oct 4;11(4):97
- Who.int/health-topics/anaemia
- Bertani L. et al., “Oral Sucrosomial® Iron Is as Effective as Intravenous Ferric Carboxy-Maltose in Treating Anemia in Patients with Ulcerative Colitis”, Nutrients 2021 Feb 12;13(2):608.doi:10.3390
- Mahadev, et al., “Prevalence of Celiac Disease in Patients with Iron Deficiency Anemia – a Systematic Review with Meta-analysis”, Gastroenterology. 2018 Aug; 155(2): 374–382.e1
anemia Carenza di ferro minerali ricerca scientifica sucrosomiale
